Legionella compliance has become a central concern for many facilities as awareness of waterborne pathogens continues to grow. Legionella bacteria, including Legionella pneumophila, can colonize building water systems and create conditions that lead to Legionnaires disease, a severe form of pneumonia. For building owners and operators, managing this risk is no longer optional. It is closely tied to regulatory compliance, health and safety obligations, and protecting public health.
While the federal government does not impose a single nationwide Legionella law, standards, regulations, and enforcement expectations increasingly require documented prevention strategies. Healthcare facilities, long term care facilities, nursing homes, and other high-risk environments face particular scrutiny. However, commercial and institutional facilities of many types are also expected to demonstrate proactive risk management.
Understanding legionella compliance means more than performing occasional testing. It involves identifying hazardous conditions, implementing structured control strategies, and maintaining documentation that shows an organization’s commitment to disease prevention. This article outlines the regulatory landscape, technical requirements, and practical steps facilities must consider to manage Legionella risks responsibly and defensibly.
What Legionella Is and Why It Matters
Legionella is a genus of bacteria commonly found in natural freshwater environments. In manmade building water systems, however, legionella bacteria can multiply to levels that create significant health concerns. The species most frequently associated with disease is Legionella pneumophila, which can cause Legionnaires disease when inhaled through contaminated aerosols.
Legionella contamination becomes a serious public health issue when water droplets containing the bacteria are dispersed into the air and inhaled. Unlike many other waterborne pathogens, infection does not typically occur from drinking contaminated water. Instead, exposure is linked to inhalation from showers, faucets, decorative fountains, hot tubs, and cooling tower drift.
Where Legionella Grows in Water Systems
Legionella growth is influenced by environmental and operational conditions inside building water systems. Certain system characteristics increase the likelihood of bacterial amplification.

Common risk areas include:
- Stagnant water in oversized or underused piping
- Dead legs and low-flow sections
- Inadequately maintained storage tanks
- Cold water storage tanks with insufficient turnover
- Warm temperatures in hot and cold water distribution
- Reduced disinfectant residual or fluctuating disinfectant levels
- Biofilm, scale, and sediment accumulation
Both hot and cold water systems can support legionella growth when conditions allow. Hot water that is not maintained at proper temperature control levels can fall into the growth range. Similarly, cold water systems that warm above recommended thresholds can become vulnerable.
How Exposure Occurs
Legionella spreads when contaminated water becomes aerosolized. High-risk sources often include:
- Cooling tower systems
- Decorative fountains
- Hot tubs and spas
- Showers and spray fixtures
These systems create fine droplets that can carry legionella pneumophila deep into the lungs. If hazardous conditions are present within the system, the risk of contamination and subsequent disease increases.
Because building water systems are complex and interconnected, understanding where growth and spread may occur is foundational to effective legionella prevention and long-term risk management.
Regulatory Framework Governing Legionella Compliance
Facilities often ask a simple question, “What are we required to do?” In practice, legionella compliance is shaped by a combination of consensus standards, public health guidance, healthcare oversight expectations, and state regulations. Even when a specific activity is not mandated everywhere, many facilities are expected to demonstrate that they have evaluated legionella risks and implemented a defensible prevention approach.
Major Standards and Guidance Commonly Used for Compliance
In the United States, the most widely referenced framework for legionella risk management is ASHRAE Standard 188, which outlines how to develop and maintain a water management program for building water systems. Many organizations use ASHRAE 188 as the backbone for decision-making because it defines how to identify hazardous conditions, establish control measures, and document ongoing management.
Public health agencies also provide guidance that influences compliance expectations. The Centers for Disease Control and Prevention (CDC) offers practical tools for building an effective water management program, including guidance on assembling a team, mapping water systems, setting control limits, and implementing corrective actions. Facilities frequently rely on these resources when building internal programs, responding to public health questions, or demonstrating an organization’s commitment to protecting public health.
Compliance Expectations at a Glance
| Framework or Authority | Where It Applies Most | What It Typically Expects | Why It Matters |
|---|---|---|---|
| ASHRAE 188 | Many building water systems | Risk-based program development, monitoring, documentation | Common benchmark for defensible compliance |
| Public health guidance (CDC) | Broad facility types | Practical steps to manage legionella risks | Often referenced during investigations and reviews |
| Healthcare oversight (CMS and related bodies) | Healthcare facilities | Policies, procedures, and implementation to manage risk | Strong driver of regulatory compliance in healthcare |
| State regulations and local requirements | Varies by state | Cooling tower rules, documentation, inspections, testing | Requirements can be enforceable and time-sensitive |
Healthcare Facilities and CMS-Driven Expectations
Healthcare facilities face heightened risk due to vulnerable populations and complex water systems. In many healthcare settings, oversight expectations emphasize infection prevention and documented water management. This can include hospitals, critical access hospitals, and long term care facilities such as nursing homes. Because these facilities may be subject to Medicare and Medicaid services participation requirements, they often need written policies and procedures that demonstrate legionella prevention and risk management.
State Regulations and Local Enforcement
State regulations can add specific requirements, especially for cooling tower programs. Some jurisdictions require registration, routine maintenance and reporting, and documented risk assessments, while others rely more heavily on established standards and public health guidance. Because requirements vary by location and can change over time, facilities should treat legionella compliance as a living program. It should be reviewed regularly and updated when building water systems, usage patterns, or regulatory expectations change.
Core Components of an Effective Water Management Program
A structured and well-documented water management program is the foundation of legionella compliance. Rather than relying solely on periodic testing, an effective water management program focuses on identifying risk, implementing control measures, and maintaining continuous oversight of building water systems.
The goal is not only to respond to contamination, but to manage legionella proactively through systematic risk management and prevention strategies.
Program Leadership and Organizational Commitment
An effective water management program begins with clear leadership and defined responsibilities. This demonstrates an organization’s commitment to health and safety.
Key elements include:
- Designating a responsible team with authority to make decisions
- Defining roles for operations, maintenance, infection prevention, and safety personnel
- Documenting procedures and accountability
- Ensuring staff understand how to conduct required monitoring and respond to hazardous conditions
Without defined leadership, even well-designed programs can fail during implementation.
System Mapping and Legionella Risk Assessments
The next step is understanding how water moves through the building. Facilities should map all relevant building water systems, including potable water systems, cooling tower systems, decorative fountains, hot tubs, storage tanks, and other components.
A thorough evaluation includes:
- Conducting legionella risk assessments for each system
- Identifying areas of stagnant water, dead legs, and low-flow sections
- Evaluating hot and cold water temperature ranges
- Assessing disinfectant residual stability and disinfectant levels
- Reviewing equipment such as mixing valves and water softeners that may influence conditions
These risk assessments form the basis of legionella risk management decisions and guide the selection of appropriate control measures.
Control Measures and Control Limits
Once risk areas are identified, facilities must define how they will control legionella growth.
Control measures often include:
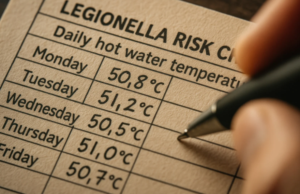
- Temperature control in hot water and cold water systems
- Maintaining appropriate disinfectant residual
- Routine flushing of infrequently used outlets
- Physical cleaning and scale removal
- Biocide application in cooling tower systems
For each control measure, facilities establish measurable control limits. For example, acceptable temperature ranges or disinfectant levels are documented as thresholds that must be maintained.
These limits allow operators to identify deviations quickly and reduce the likelihood of legionella contamination.
Monitoring, Verification, and Validation
Monitoring ensures that control measures remain effective over time. This may include:
- Recording temperature readings in hot and cold water systems
- Measuring disinfectant residual regularly
- Performing routine inspection and maintenance
- Conducting periodic testing and reviewing sampling results
Verification confirms that the program is being implemented as written. Validation, which may include targeted testing for legionella bacteria, helps determine whether the program is effectively controlling risk.
Testing should be part of a broader strategy, not the sole method of prevention.
Documentation and Corrective Actions
Documentation is essential for regulatory compliance and legal defensibility. Facilities should maintain records that include:
- Risk assessments and system maps
- Defined control measures and control limits
- Monitoring logs
- Testing data and sampling results
- Documented corrective actions when deviations occur
When monitoring shows that a control limit has been exceeded, facilities must take clearly defined corrective actions. These following actions may include system disinfection, flushing, adjustment of temperature, or other remediation steps.
A comprehensive, documented approach supports legionella prevention, demonstrates due diligence, and strengthens overall compliance efforts.
Critical Risk Areas Within Water Systems
Even with a documented water management program, certain components of building water systems require closer attention. These areas often present elevated legionella risks due to temperature fluctuations, stagnant water, or inconsistent disinfectant residual.
Understanding where problems typically develop allows facilities to prioritize inspection, maintenance, and monitoring efforts.
Potable Hot Water Systems
Potable water systems, particularly hot water distribution, are among the most common areas associated with legionella growth.
Risk factors in hot water systems include:
- Inadequate temperature control
- Heat loss in long distribution loops
- Improperly balanced recirculation systems
- Mixing valves that reduce temperature below protective thresholds
- Biofilm or scale buildup in storage tanks
If hot water temperatures drop into ranges that promote bacterial growth, the risk of legionella contamination increases. Maintaining consistent hot temperatures, while balancing scald prevention requirements, is a core part of legionella control.
Facilities must also ensure that disinfectant levels remain stable throughout the distribution network, especially at distal outlets.
Cold Water Systems and Cold Water Storage Tanks
Cold water systems are often overlooked, yet they can contribute significantly to legionella growth when temperatures rise or water becomes stagnant.
Common concerns include:
- Cold water storage tanks exposed to ambient heat
- Poor insulation allowing temperature elevation
- Limited turnover in oversized storage tanks
- Stagnant water in dead legs or underutilized branches
- Depleted disinfectant residual
Cold water that warms above recommended thresholds can create favorable conditions for bacteria. Regular inspection, turnover management, and maintenance of storage tanks are essential components of prevention.
Fixtures, Devices, and Point-of-Use Considerations
Fixtures and endpoint devices can influence overall system performance and may create localized hazardous conditions.
Examples include:
- Point of use filters that require scheduled replacement
- Mixing valves that blend hot and cold water
- Shower heads and faucet aerators that accumulate biofilm
- Water softeners that alter disinfectant dynamics
If maintenance schedules are not followed, these components may contribute to reduced disinfectant levels or increased stagnation.
Design and Operational Contributors to Risk
Beyond specific equipment, broader system characteristics can increase risk:
- Complex or oversized building water systems
- Areas with low occupancy and stagnant water
- Infrequent flushing in sections of the system
- Inconsistent maintenance practices
Addressing these contributors requires coordination between facilities management, health and safety teams, and water treatment professionals. By focusing on high-risk areas and maintaining disciplined oversight, facilities strengthen both prevention and long-term compliance efforts.
Cooling Towers and High Risk Equipment
Among all building water systems, the cooling tower is one of the most closely scrutinized components in legionella prevention efforts. Cooling towers can generate fine aerosol droplets, which increases the potential for legionella bacteria to spread beyond the immediate system if growth is not properly controlled.
Because of this elevated risk, cooling tower programs are often specifically addressed in state regulations and public health guidance.
Why Cooling Towers Present Elevated Risk
Cooling towers create conditions that may support legionella growth if not properly maintained:
- Warm circulating water that supports bacteria
- Nutrient accumulation from environmental debris
- Biofilm formation on internal surfaces
- Variable disinfectant residual
- Continuous aerosol generation
If legionella contamination develops in a cooling tower system, the potential for offsite impact increases due to airborne drift. This makes consistent maintenance and structured oversight essential for both safety and compliance.
Typical Control Approach
A structured cooling tower program typically includes:
- Routine inspection and mechanical maintenance
- Scheduled cleaning to remove scale, sediment, and biofilm
- Application of appropriate biocide treatment
- Monitoring of disinfectant levels and system performance
- Defined control limits for key operational parameters
Water treatment programs are often central to controlling growth and maintaining system stability. Effective legionella control in cooling towers depends on consistent implementation rather than reactive intervention.
Testing and Response Considerations
Many facilities incorporate periodic testing as part of their overall strategy. Testing should be used to validate performance, not replace routine maintenance and chemical control.
If sampling results indicate elevated bacteria levels, facilities must follow predetermined corrective actions. These following actions may include additional cleaning, adjustment of treatment programs, system disinfection, or temporary shutdown when necessary.
By maintaining disciplined oversight of cooling towers and other high-risk equipment, facilities reduce the likelihood of growth, limit contamination, and strengthen overall legionella prevention efforts.
Consequences of Non-Compliance
Failure to maintain an effective program for legionella compliance can expose facilities to operational, legal, and reputational consequences. Because Legionella is associated with serious disease and public health impact, enforcement agencies and oversight bodies tend to scrutinize prevention efforts closely after an incident.
When a case of Legionnaires disease is linked to a facility, investigations often focus on whether appropriate risk management practices were in place. Regulators may review documentation, monitoring logs, risk assessments, and corrective actions to determine whether reasonable steps were taken to protect health and safety.
Potential consequences of inadequate compliance include:
- Regulatory citations or mandated corrective measures
- Increased oversight from health departments or other authorities
- Disruption of operations during remediation
- Legal claims or litigation exposure
- Reputational damage that affects tenant or patient confidence
For healthcare facilities and other high-risk environments, scrutiny can be especially significant due to vulnerable populations and infection prevention obligations.
Beyond enforcement, the broader concern is protecting public health. Facilities that proactively manage risk demonstrate a commitment to safety and responsible operation. In contrast, reactive approaches can increase liability and undermine trust.
A structured and well-documented approach to legionella compliance strengthens both prevention and defensibility, reducing risk while supporting long-term operational stability.
How ETI Supports Water Treatment Professionals in Legionella Risk Management
Effective legionella compliance depends not only on facility operations, but also on the technical strength behind the water treatment program. For independent water treatment professionals, delivering defensible programs requires reliable chemistry, regulatory awareness, and access to technical expertise.
Eastern Technologies, Inc. (ETI), a 2023 AWT Supplier of the Year and ISO certified manufacturer and distributor, exists to support water treatment professionals without competing with them. As a proud AWT member with more than 38 years of industry experience, ETI operates under a clear commitment: Supporting Water Treatment Professionals.

Technical Expertise and Program Support
Legionella risk management programs require more than product supply. They require sound application guidance and troubleshooting support.
ETI provides:
- Access to a technical team with decades of combined experience
- Guidance on selecting appropriate control measures for cooling towers and potable systems
- Support interpreting sampling results and adjusting treatment strategies
- Assistance navigating compliance considerations and documentation practices
This technical partnership allows water treatment professionals to manage legionella proactively and respond confidently when conditions change.
Chemistry Breadth and Application Guidance
Effective legionella control often requires flexibility. Different systems, materials, discharge limitations, and local regulations may influence treatment decisions.
ETI supports this need through:
- A broad portfolio of oxidizing and non-oxidizing biocides
- Custom formulation capabilities
- Private label and manufacturer label options
- EPA supplemental registration assistance when needed
This flexibility helps professionals tailor water management strategies to the specific risk profile of each facility while maintaining consistent compliance standards.
Operational Reliability and Documentation Support
In compliance-driven environments, reliability matters. Inconsistent supply, incomplete paperwork, or formulation variability can create unnecessary risk.
ETI’s quality-focused operational approach emphasizes:
- Consistent product quality
- Accurate documentation
- Reliable order fulfillment
- Support resources available through a 24/7 distributor portal
For water treatment professionals building defensible programs, having a dependable partner behind the scenes strengthens both risk management and regulatory compliance efforts.
To learn more about ETI’s biocide portfolio and technical support resources, contact us today.
Frequently Asked Questions (FAQs)
What are the OSHA guidelines for Legionella?
OSHA does not have a specific standalone Legionella standard, but it references Legionella under its General Duty Clause, which requires employers to provide a workplace free from recognized hazards. OSHA has issued technical guidance documents that outline prevention strategies, including maintaining water systems, temperature control, and appropriate disinfectant levels. Employers are expected to assess potential Legionella risks and implement reasonable control measures to protect worker health and safety.
What exactly is Legionella?
Legionella is a type of bacteria found naturally in freshwater environments that can grow in building water systems under certain conditions. The species Legionella pneumophila is most commonly associated with Legionnaires’ disease, a serious form of pneumonia. Infection typically occurs when individuals inhale aerosolized water droplets containing the bacteria, rather than from drinking contaminated water.
Do you legally have to have a Legionella risk assessment?
Whether a Legionella risk assessment is legally required depends on the jurisdiction and facility type. Some state regulations mandate documented risk assessments, particularly for cooling tower systems. In healthcare facilities and other regulated environments, oversight bodies may expect formal evaluations as part of broader compliance obligations. Even where not explicitly mandated, conducting risk assessments is widely recognized as a best practice for effective Legionella risk management.
What are the Legionella regulations?
There is no single federal law that governs all Legionella prevention activities in the United States. Instead, regulations are shaped by a combination of ASHRAE standards, public health guidance, healthcare oversight requirements, and state-specific rules. Certain states have enforceable cooling tower regulations, while healthcare facilities may face additional expectations tied to Medicare and Medicaid services participation. Because requirements vary, facilities should review applicable local and state regulations and maintain a documented water management program to support compliance.